The pharmaceutical struggle
With the COVID-19 pandemic still accelerating across the globe, it is painfully clear that the pharmaceutical sector is failing to find fast, reliable solutions for diagnostics, prevention, and treatment, that are deployable at scale. This issue is not new, nor uniquely linked to COVID-19. It's a fundamental, widespread shortcoming that only became more visible by the augmenting effect of the pandemic. For at least two decades, the pharma sector has made increasing investments in R&D yet has produced drastically fewer new molecules. The shortage of good medicines in the pipeline underlies many of the other challenges pharma faces, including its increasing expenditure on sales and marketing, competition from start-ups, deteriorating financial performance, and damaged reputation.
Today, pharma’s challenge is to develop new medicines that can prevent or cure diseases that are currently considered incurable. On top of this challenge, healthcare is becoming increasingly personalized. We are moving away from 'one size fits all' diagnostics and medicines and moving towards increased attention on each individual patient's context and (genetic) disposition. In other words, if 'Mary' gets cancer, she will no longer be given a standard cocktail of chemical and radiation therapy, but instead, she’ll receive a fine-tuned treatment optimized to what will most likely work for her individual situation. Think COVID-19 versus baby Pia. COVID is an acute urgency that hit all of us globally in a similar way. Baby Pia, the baby diagnosed with a rare spinal disease, who needed a very (€1.9m) expensive medication in order to live, embodies the need for more personalized healthcare and the human right to receive medical treatment, regardless of how rare (and therefore economically uninteresting to pharma) your condition might be.

Paradigm shift in the pharmaceutical sector, moving to a patient-centric industry (source: Arthur D. Little, The Future of Healthcare 2017)
By using the traditional discovery and development processes, even when multiplying them thanks to sudden (crisis-inspired) investments as we see now with COVID, there is little reason to think pharma's underlying efficacy and productivity will magically rise. An additional innovative pathway should focus on accelerating R&D with technology and operational efficiencies, through extended collaboration with other biopharma companies, smaller biotech companies, research institutions, and academia.
Nanoelectronics and artificial intelligence to the rescue
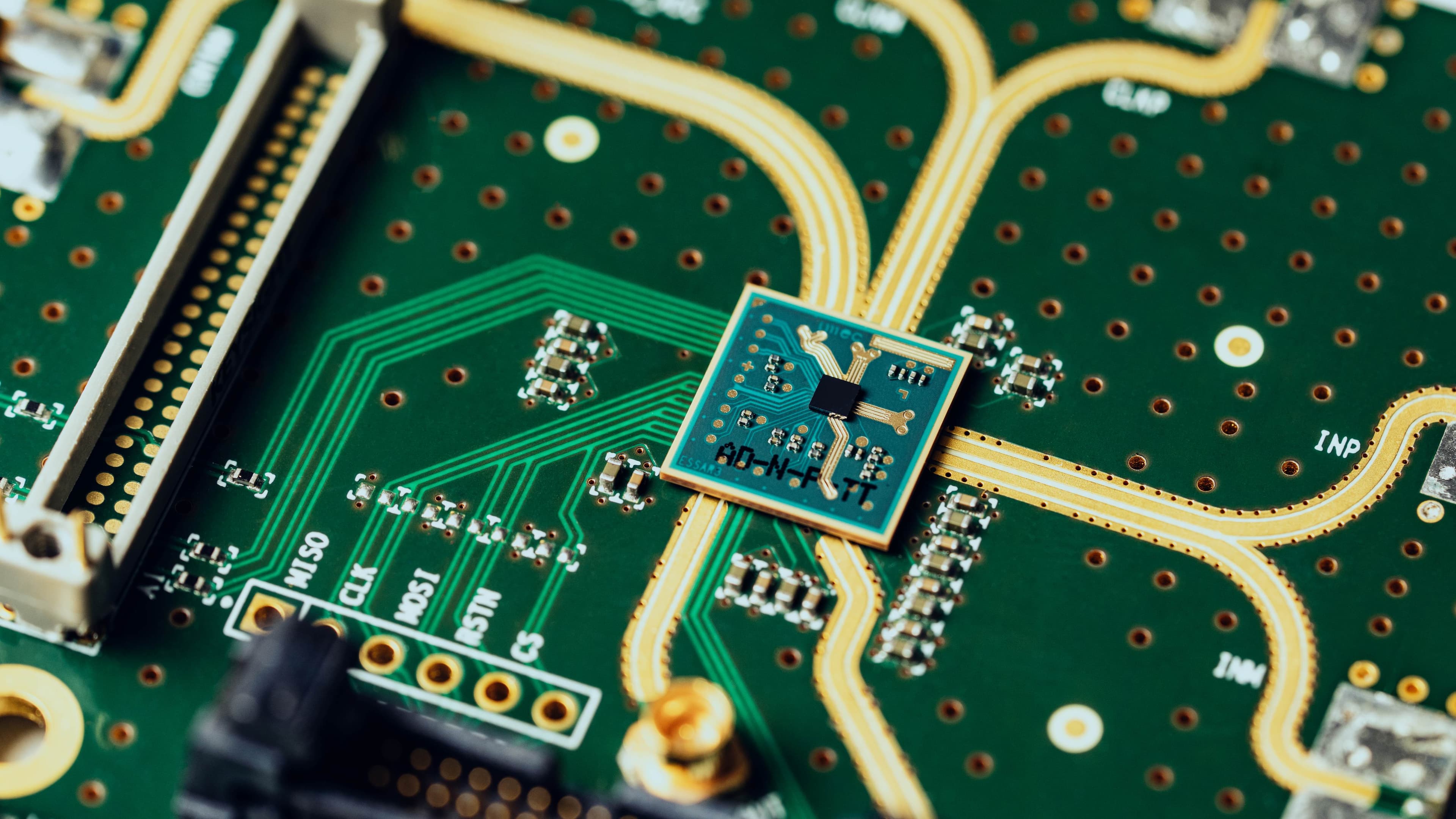
To increase R&D efficiency at lower cost, the pharma industry needs to transit towards less hands-on and more automated processes. Think of advanced nanoelectronics lab-on-chip prototypes that are capable of running an unprecedented number of tests in parallel on a scalable miniaturized device. Or imagine combining multiple types of data gathered at different places in the discovery process to create a knowledge database from which advanced data algorithms can identify and prioritize candidates more optimally and dynamically throughout the process. And how about artificial organs? Or more individualized patient models supported by AI and deep learning? Thanks to these advances, a higher throughput can be obtained in screening and making the right selection of products that will hold up during consecutive trials. In the context of these clinical trials, a whole new set of challenges pops up. Recruiting and screening patients is already a time-consuming process. In fact, a 2018 study by CB insights shows that 80 percent of clinical trials fail to meet enrollment times because of the process alone. Then once they finally get started, following up on patients' compliance with, and responses to the protocols are also cumbersome activities. Oftentimes, they still involve error-prone written diaries and are conducted in expensive, highly controlled environments. To top it off, third parties increasingly require undisputable proof of efficacy for a drug to be reimbursed. The pharma industry is responding by pursuing trials that collect real-world evidence in the participants' daily environment. Wearables and AI-driven data analytics are two of the key enabling technologies behind these new types of trials. Although both have moved beyond the hype and gadget stage, they still face significant reluctance from the pharma industry. The next generation of point-of-care sensors and digital biomarkers currently under development will add a new layer of information that might make clinical trials and individualized trajectories even more precise. So, once the sector overcomes its fears, it will notice that these technologies enable an acceleration of products successfully coming out of trials and moving into production.

An illustration of the variety and complexity of datasets as they are fed into big-data analytics and artificial intelligence engines for assisted decision-making in a medical context.
Once in the manufacturing stage, yield and contamination control are amongst the key parameters being monitored. Inside the bioreactors, and during upstream and downstream handling, it is vital to prevent undesired biological material (foreign DNA, bacteria, etc.) from entering the production flow. Typically, this bioburden, as it is called, is monitored by taking samples and testing them with high-end analytical tools, either offline in a laboratory or at-line near the production line. Here again, nanoelectronics-based devices, like DNA or ion sensors and on-chip or lens-free microscopes, are orders of magnitude more compact, significantly cheaper, and can be deployed in a more integrated way with the process flow itself. These state-of-the-art technologies also enable online monitoring and don’t affect the monitored product: two benefits that become even more important in the growing domain of personalized cell therapies, where each patient has its own associated bioreactor. This advanced personalization also means quantities are low and cost is dominated by the long turnaround time, largely resulting from the hands-on time spent on necessary testing. While the needle-to-needle time from blood extraction to the start of the treatment should in fact be as short as possible to save more lives.

Chip technology is mature enough to shift the focus of process analytical technologies for complex analyses (e.g. bioburden: cells, DNA, proteins, ions, etc.) towards at-line, on-line and inline testing.
Partnerships and disruption
All of the above advancements could be sorted into short-to-mid-term incremental innovations with mature technologies behind them, waiting to be implemented. Then when we allow ourselves to dream further into the future, there's a myriad of additional synergies between nanoelectronics and pharma to discover. Think of a 'digital twin' that could profile a patients’ behavior and context in a virtual environment as an additional layer of biometric-phenotyping information aside from its genetic map. Potentially completed with organ-on-chip devices such as on-chip artificial hearts or lungs to create functional models on which simulations could be run before implementing a drug or therapy in real life. Significant progress is also being made in the domain of ingestibles: miniaturized electronic devices that can be swallowed, and perform sensing and actuation in ‘our natural bioreactor’ (the digestive tract). And genomics, where nanoelectronics could provide the means to increase precision and throughputs while lowering costs for genetic mapping and engineering. We could even move to the next level of non-drug-based treatments like electrical (vagus) nerve stimulation, which could prevent people from having to take certain drugs or even allow the creation of a fully bionic replacement organ.
These and most other disruptive scenarios are currently in the playground of universities and research institutes, spin-offs, and startups. In Belgium, significant progress is happening with involvement from imec, UZ Gasthuisberg Leuven, VIB and their spinoffs. Notably, ULB (Université Libre de Bruxelles) has a biotech center in Charleroi, and a vibrant startup ecosystem that emerged around it as a result of several successful spinoffs. In other words, all of the ingredients to build successful synergies and partnerships exist an area smaller than Silicon Valley. This is one of the reasons I am most excited and optimistic about the future synergies between the technology and pharma sector. My optimism is fed by the observation that attitudes have started to change over the last few years. Until recently, my colleagues and I felt like missionaries, traveling around, preaching our research’s potential value to industry stakeholders. We knew we had reached an important milestone when pharmaceutical companies began to approach us proactively. Over the last couple of years, many pharmaceutical companies have visited imec to learn about our latest developments and projected roadmaps in nanoelectronics for life sciences, and we are finally landing the first contracts. The whole medical community is gradually acknowledging the importance of digital health. The pharmaceutical sector often finds it difficult to capitalize on these opportunities and will continue to do so unless it can change the way it functions. Digitization, along with intelligent automation in manufacturing, and establishing the right partnerships, can eventually help companies reduce their go-to-market cycle for drugs.

Liesbet Lagae is imec Fellow and co-founder and Program Director of the Life Science Technologies in imec. In this role, she oversees the emerging R&D, the public funded activities and early business creation. She holds a PhD degree from the KU Leuven, Belgium for her work on Magnetic Random Access Memories. As a young group leader, she has initiated the field of molecular and cellular biochips leveraging silicon technologies at imec, Belgium. The life science program has grown from emerging activities to a mature business line that provides smart silicon chip solutions to the life science industry. Applications include medical diagnostics, point-of-care solutions, DNA sequencing, cytometry, bioreactors, neuroprobes, implants. She holds a prestigious ERC consolidator grant for developing a platform on single cell analysis and sorting. She has (co-) authored 125 peer-reviewed papers in international journals and holds 15 patents in the field. She is also part-time professor in nanobiotechnology at KU Leuven/Physics department.
More about these topics:
Published on:
30 September 2020